News Story
Bastopcu and Ulukus build model for real-time timely tracking of COVID-19 infection and recovery
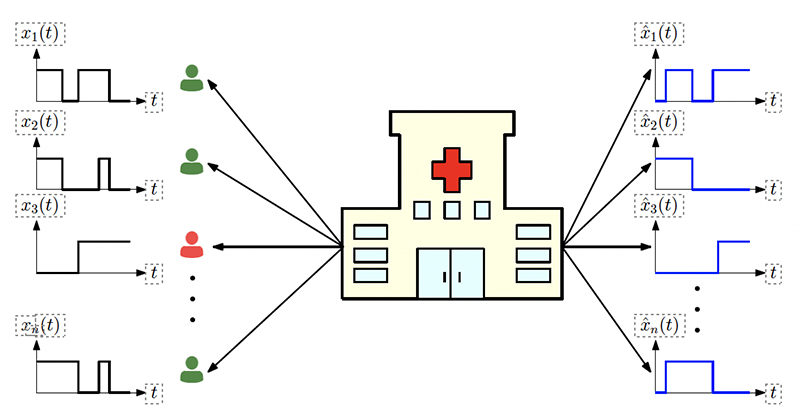
Figure 1 from the paper. The system model illustrates n people whose infection status are given by xi(t). The health care provider applies tests on these people. Based on the test results, estimations for the infection status xˆi(t) are generated. Infected people are shown in red and healthy people are shown in green.
A new model built by alumnus Melih Bastopcu (ECE Ph.D. 2021), a postdoctoral researcher in the Coordinated Science Laboratory, University of Illinois Urbana-Champaign; and his former advisor Professor Sennur Ulukus (ECE/ISR) considers real-time timely tracking of infection status of COVID-19 of individuals in a population.
In Using Timeliness in Tracking Infections, Bastopcu and Ulukus construct a model that considers the situation of a health care provider who wants to quickly detect both infected and recovered people. Obviously the provider wants to detect infected people as quickly as possible so that precautions such as isolating them from the rest of the population can be taken. The provider also wants to be able to detect people who have recovered from the disease as soon as possible so they can return to work.
To measure the tracking process’s timeliness, Bastopcu and Ulukus use the long-term average difference between the actual infection status of people and the health care provider’s real-time estimate based on the most recent test results.
They find an analytical expression for this average difference for given test rates, infection rates and recovery rates. Then they propose an alternating minimization based algorithm to find the test rates that minimize the average difference. If the total test rate is limited, instead of testing all members of the population equally, only a portion of the population may be tested in unequal rates calculated based on their infection and recovery rates.
The researchers characterize the average difference when the test measurements are erroneous (aka “noisy”). They also consider cases where the infection status of individuals may be dependent, which happens when an infected person spreads the disease to another person if they are not detected and isolated by the health care provider.
In addition, Bastopcu and Ulukus consider an age of incorrect information-based error metric where the health care provider does not detect the changes in people’s infection status for a period of time. This “staleness metric” increases linearly over time. Through extensive numerical results, the researchers observe that increasing the total test rate helps in tracking infection status. In addition, an increased population size increases diversity of people with different infection and recovery rates. This may be exploited to spend testing capacity more efficiently, thereby improving the system performance.
Depending on the health care provider’s preferences, the model can adjust test rate allocation to detect either infected people or recovered people more quickly. When there are errors in the tests, it may be more advantageous for the health care provider not to test everyone, and instead, apply more tests to a selected portion of the population.
In the case of people with dependent infection status, as the model increases the total test rate, the health care provider detects the infected people more quickly, and thus, the average time that a person stays infected decreases. Finally, the researchers note the error metric needs to be chosen carefully to meet the priorities of the health care provider, as the error metric used greatly influences who will be tested and at what test rates.
Published April 19, 2022