News Story
New model for U.S. liver transplant allocation could reduce disparities, save lives
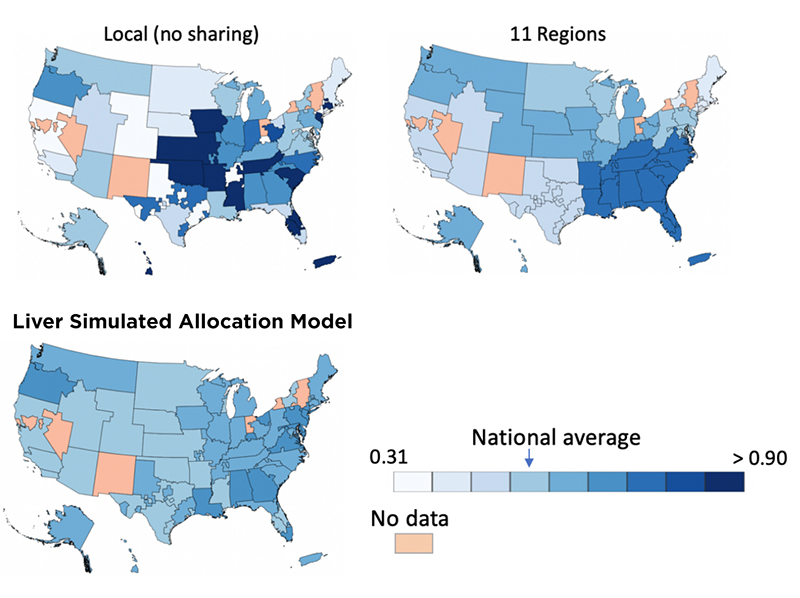
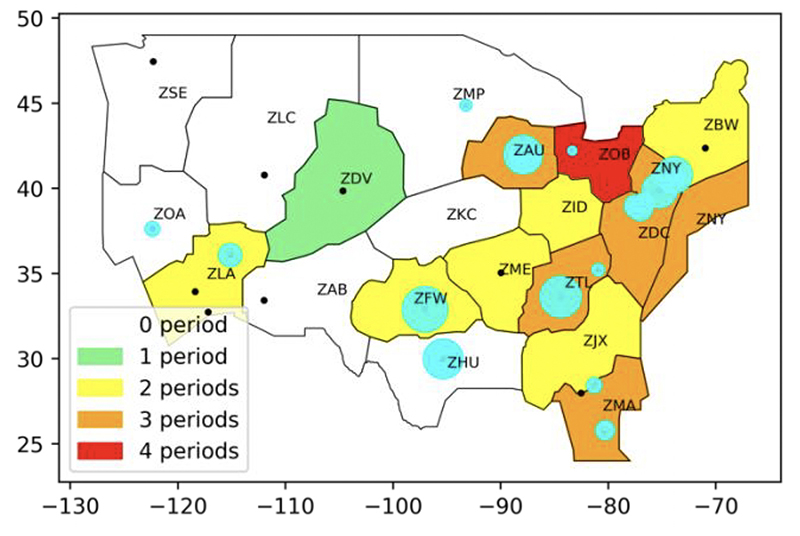
[Click for larger image] The optimized scheme of the Liver Simulated Allocation Model (bottom) reduces the inherent supply/demand ratio disparity of the DSAs compared to no sharing at all (top left) and the current "11 Region" model (top right). Lighter blue = less disparity; darker blue = more disparity. (Modified Fig. 7 from the paper)
Many long-standing criticisms of how organ transplants are handled in the United States center on how potential recipients are queued for the opportunity to receive a donated organ, and how the waiting time varies by where one lives in the country.
To design a fairer system that could reduce inequities, Professor S. Raghu Raghavan (Smith School of Business/ISR); his Ph.D. student Shubham Akshat; and Sommer Gentry a professor in the U.S. Naval Academy’s Department of Mathematics and a research associate in surgery at the Johns Hopkins School of Medicine; have developed a nonlinear integer programming model that allocates deceased donor livers to maximize minimum supply/demand ratios across all transplant centers.
Their paper, Fair Liver Transplant Allocation: A Scalable Optimization Model, reformulates the current allocation situation as a set-partitioning problem, enabling scaling to more granular geographical units. The new model matches supply and demand in a more equitable fashion than existing and proposed policies; and holds significant potential to improve the liver transplantation landscape, potentially saving 340 lives on average over a period of four years.
The current problem
Geographical disparity is tied to wide variations in supply/demand ratios (organ supply to patient demand) across the country. Liver transplants are a good example of how demand outstrips supply. In 2018, more than 13,000 patients in the United States were on the waiting list for a liver transplant, while 8,250 liver transplants took place. On average, three Americans awaiting a liver transplant died every day; a total of 1,155 lives were lost this way in 2018.
U.S. law designates deceased donor organs as national resources, and the federal government uses the Organ Procurement and Transplantation Network (OPTN) to coordinate the nationwide transplant system and optimize the use of donor organs. The United Network for Organ Sharing (UNOS), a non-profit private organization, oversees the OPTN. It follows the “Final Rule,” a detailed regulatory framework that requires policies shall not be based on where a candidate lives or is listed, except to the extent required by the other requirements of the Rule.
The country’s current allocation policy divides the U.S. into 11 regions. Smaller units, called Donation Service Areas (DSAs), fit roughly, but not perfectly, within the 11 regions. [CLICK HERE to see an image of the 11 regions and the DSAs] Livers are offered to patients within a DSA in decreasing order of medical urgency. This is measured by a score called the Model for End-stage Liver Disease (MELD). The MELD score reflects the probability of death within a 3-month period and ranges from 6 to 40; the higher the score, the greater the mortality risk. The most serious patients are assigned Status 1A and 1B; the number is fewer than 50 nationwide at any time.
This complicated existing system has many weaknesses and is widely regarded as unfair. Indeed, numerous lawsuits over the years charge that the division into regions and DSAs can result in a person with a high MELD score being penalized when a nearby organ becomes available because they live close to—but not in—the DSA or regional boundary where the organ is located. In addition, there is wide geographic variation in median MELD scores. The main problem is that patients receiving organs may be both less sick and more geographically distant than a patient with higher medical priority.
In response, UNOS has asked researchers to develop new frameworks based on three criteria: fixed distance from the donor hospital, mathematically optimized boundaries, and continuous distribution where candidates are ranked by a combination of their medical urgency and proximity to a donor.
The Liver Simulated Allocation Model
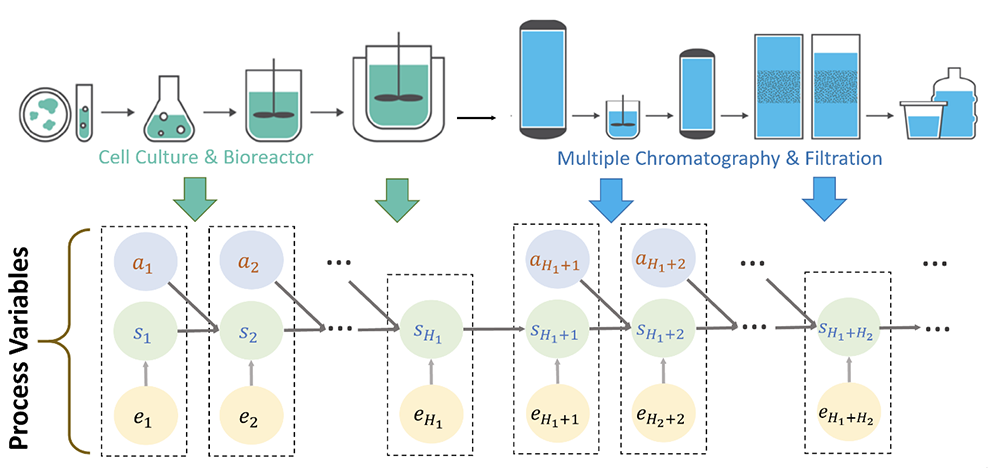
Believing equalizing supply/demand ratios is the key to address geographical disparity, the authors sought to build a general methodology based on overlapping areas (“neighborhoods”). Because mathematical optimization is better able to equalize the supply/demand ratio at transplant centers than the schemes used in existing frameworks, the authors use this method to design heterogeneous-sized areas around donation locations.
The authors abide by the maximin principle that the least well-off group in the society should be made as well off as possible to improve the situation of the geographical area with worst access to organs. They solve for cases where DSAs and zip-code clusters are the geographical units and use supply/demand ratios as the metric to define access.
To remedy the current situation of non-overlapping regions, the authors carefully defined the supply/demand ratio. Using a Mixed-Integer Programming optimization model, they first maximized the minimum supply/demand ratio across the geographies. Then, they minimized the maximum absolute difference of supply/demand ratio among nearby areas and the maximum supply/demand ratio across all geographies.
The authors then ran simulations with historical patient and organ donor data to compare their new optimized geographical schemes with the current 11-region scheme on metrics like the variance of Median MELD at Transplant, the number of deaths incurred, and the distance traveled.
They found their new Liver Simulated Allocation Model significantly improves the worst supply to demand ratio across transplant centers. The new geographical distribution scheme reduces the variance of average distance traveled by a factor of three, drastically reduces the variance of Median MELD at Transplant (which measures inequities) from 7.26 to 1.61, and could save 340 lives on average over a period of 4 years.
“We hope this research will spur similar work in other organ transplantation settings,” the authors write, “and will help to reduce and mitigate the geographical disparities that are inherent to all of these systems.”
Published May 19, 2020